Imaging

Soft tissue and skeletal injuries are of significant concern in sport horses. Fortunately, veterinary knowledge and technology are rapidly advancing to quickly and accurately diagnose and treat such issues. Medical imaging technologies, including digital radiography (X-ray), computerized tomography (CT), magnetic resonance imaging (MRI), ultrasonography, scintigraphy (bone scan), and positron emission tomography (PET) have become powerful diagnostic tools. Each approach has its own strengths and weaknesses, but the modalities are often successfully used in combination with one another to accurately facilitate diagnosis and direct appropriate treatment.
Radiography (X-rays) and ultrasound have historically been the main diagnostic imaging tools available in equine veterinary practice. As the technologies evolved, image processing became more advanced and systems have become easily portable, changing the way imaging is performed in the field. Advanced imaging systems, such as computed tomography (CT) and magnetic resonance imaging (MRI) are commonly used in veterinary hospital settings, along with nuclear scintigraphy (bone scan). Most recently, positron emission tomography (PET) has become available in the horse. Radiography, ultrasound and CT scans generally reflect changes to form or structure (morphologic changes). Nuclear scintigraphy and PET, on the other hand, reflect changes in the functions and mechanisms at work within an organism (physiologic changes). MRI captures both morphologic and physiologic information.
- Radiography (X-ray)
-
Radiography is commonly used for the diagnosis of skeletal injury. It is generally an affordable, portable approach that is easy for the veterinarian to use. With digital radiography, images can be captured, assessed, and additional images obtained immediately on site if needed without having to return to the clinic to process film. Radiography is not as sensitive as some of the more advanced systems, but it has a long history of successful use in diagnosing bone injuries.
Image: digital or film, 2-dimensional, reflects morphologic changes
Best for: bone
Uses: evaluate causes of lameness, detect and characterize fractures, identify arthritis, diagnose lung disease, investigate teeth and sinuses, look for ingested sand or enteroliths as causes of colic
How it works: Radiography uses a very short burst of X-rays to create an image of the body. A beam of X-rays interacts with the body and produces an image. Dense materials (like bone) absorb the radiation and show up as white areas whereas soft tissues, where the X-rays pass through, are gray or black.
How long it takes: 5 to 15 minutes depending on the region and the number of views required
Pros: affordable, portable, easy to use, does not require anesthesia
Cons: limited sensitivity, not good for diagnosing soft tissue injury
Cost: $
- Ultrasound
-
Ultrasound is commonly used to diagnose soft tissue injuries in horses. Similar to radiography, it is an affordable, portable approach that can be used in the field. First used in the field for reproductive exams, its uses have greatly expanded. Ultrasound is now used to cover a wide range of applications, including the diagnosis of tendon, ligament or joint injuries and assessment of the gastrointestinal tract in cases of acute or chronic colic. Ultrasound can be used to identify foreign bodies or fracture fragments and assist with minimally invasive removal. It can even diagnose fractures of bones that cannot be easily radiographed, such as the pelvis.
Image: digital, cross-sectional, reflects morphologic changes
Best for: soft tissue
Uses: diagnose tendon and ligament injuries, abscesses, liver disease, kidney disease, colitis, inflammatory bowel disease, cancer (or neoplasia), fractures, foreign bodies, infections, help guide therapeutic agents to joints, tendons, etc., obtain samples from organs such as liver and kidneys, masses or abscesses
How it works: High-frequency sound waves are transmitted from a transducer into the body. The transducer captures the sound waves that bounce back and a computer uses that information to create an image based on the intensity, frequency and time it takes the signal to return. For example, normal tendons are usually homogeneously bright (echogenic) and areas of injury create darker (hypoechoic) areas in comparison.
How long it takes: 45-60 minutes
Pros: comparatively inexpensive, does not require anesthesia
Cons: some areas (such as within the hoof capsule) may be difficult to fully access
Cost: $
- Computed Tomography (CT)
-
Essentially 3-dimensional radiography, CT is a quick imaging modality and can generate many cross-sectional images in seconds. Historically, general anesthesia was required since the equine patient must remain completely still during the scan. Specific scanner installation offers the option to perform standing CT of the head and neck in horses. Recently, newer technologies have led to the opportunity to image the distal limb standing; however, the image quality is not quite as high with these machines at this time.
Image: digital, 3-dimensional, reflects morphologic changes
Best for: bone, soft tissue, blood vessels
Uses: plan for surgical repair of joints and complex fractures, detailed imaging of the skulls and sinuses to plan surgery, investigate causes of seizures, diagnose causes of lameness, identify abnormal blood supply, trauma, plan radiation therapy for tumors
How it works: An X-ray tube rotates in a circle around the patient, passing a thin X-ray beam through the body. Digital detectors that are located around the circle sense the beam and produce a cross-sectional image of each “slice” of the body based on the density of tissue the X-ray beam travels through.
How long it takes: scan 10-20 minutes; including anesthesia 1-1.5 hour(s)
Pros: quick, safe procedure, 3-dimensional image, elimination of superimposition and improved contrast compared to conventional radiographs, covers larger areas than MRI in the same amount of time
Cons: not portable, requires general anesthesia, rare allergic reactions to general anesthesia or to the contrast agent, use of radiation
Cost: $$
UC Davis Diagnostic Imaging Service - Computed Tomography (CT)
- Nuclear Scintigraphy
-
Nuclear scintigraphy (a.k.a. “bone scan”) is a “functional” imaging technique, meaning that it does not assess the size and shape of structures, but rather investigates the activity of the structures being imaged. It is highly sensitive and the ideal technique to detect stress remodeling or stress fractures before radiographs can detect changes. Scintigraphy is a strong diagnostic tool when combined with other modalities.
Image: digital, 2-dimensional, reflects physiologic changes
Best for: bone, soft tissue, blood vessels
Uses: can identify cryptic causes of lameness, especially in regions difficult to image (i.e. lumbosacral spine, pelvis, etc.)
How it works: Radiopharmaceuticals are injected intravenously (IV) and a gamma camera detects the distribution of that isotope in the body. Very small, trace amounts of radioactive atoms (technetium-99m) are attached to molecules (phosphonates) that bind to bone lesions. The radiotracer collects in overactive areas of the skeleton where it gives off energy in the form of gamma rays, which are then detected by a gamma camera. A computer measures the amount of gamma rays emitted by the body in each area of interest and produces pictures that show functional details of the bones. Varying the timing of image acquisition or the radiopharmaceutical can provide information about blood vessels, soft tissue inflammation, and other problems.
How long it takes: The scan itself takes 1-2 hours, but patients must remain hospitalized for at least 24 hours in order to monitor radiation levels prior to being cleared for release.
Pros: very sensitive technique that can often diagnose diseases not visible with other imaging methods, can image large body areas
Cons: not portable, poor resolution, must have comparison between right and left symmetry and know the expected normal uptake patterns in order to interpret results
Cost: $$
- Magnetic Resonance Imaging (MRI)
-
Magnetic resonance imaging is unique among imaging modalities in that it provides both morphologic and physiologic information, whereas most others provide one or the other. It allows for visualization of soft tissue structures that cannot be seen using X-rays and is ideal for evaluating structures within the hoof that cannot be imaged by ultrasound. Images depict changes in tissue architecture and water content, such as occur with injury or inflammation, but show less detail than CT and scan times are longer than other approaches. General anesthesia is required when using a standard human MRI system, but a system was specifically designed to perform standing MRI in horses for which sedation is sufficient.
Image: digital, 3-dimensional, reflects morphologic and some physiologic changes
Best for: bone and soft tissue
Uses: identify areas of inflammation, diagnose tendon and ligament lesions (especially those within the hoof capsule), thickening of joint capsule and small bone lesions, causes of foot pain, joint inflammation, bone edema
How it works: The patient is placed in a strong primary magnetic field which lines up the North and South poles of naturally-occurring hydrogen protons in the body that are usually oriented randomly. A short duration, second magnetic field, known as the RF pulse, excites the aligned protons. The RF pulse ends after ~1 millisecond and the protons “relax” back to their previous state over several seconds under the influence of the strong primary magnetic field. The excited protons create their own magnetic field which is then detected by a coil and processed by a computer into images that show the distribution and intensity of the protons’ magnetic fields. Protons do not all relax at the same rate, so different molecules and tissues produce different signal intensities that can be used to identify normal structures and detect abnormalities within tissues.
How long it takes: 45-90 minutes per region (8-12 different individual scans providing from 8 to over 100 images per scan)
Pros: very safe procedure, no harmful effects from magnetic fields, allows visualization of soft tissue structures not seen using X-rays, useful for evaluating structures that cannot be imaged by ultrasound
Cons: not portable, requires general anesthesia (except in the case of standing MRI), prolonged scan times in comparison to other modalities, higher cost than other modalities
Cost: $$$
UC Davis Diagnostic Imaging Service - Magnetic Resonance Imaging (MRI)
- Positron Emission Tomography (PET)
-
Positron emission tomography is the latest imaging modality to become available in equine veterinary medicine. A nuclear medicine technique similar to scintigraphy, PET reflects physiologic changes but displays the results in three dimensions with increased anatomical accuracy. Depending on the radiotracer used, information can be collected regarding either bone or soft tissue. Patients most likely to benefit from PET imaging include cases in which causes for lameness are not identified with other modalities, or those in which multiple lesions are identified and it is uncertain which one is causing the lameness. UC Davis was the first veterinary institute in the world to use this imaging technology for equine patients and was the first institution to offer PET scans to clinical equine patients. UC Davis also completed the first standing equine PET scans, which eliminate the need for patients to be under general anesthesia, thereby promising to open many new clinical applications of PET in the evaluation of equine lameness.
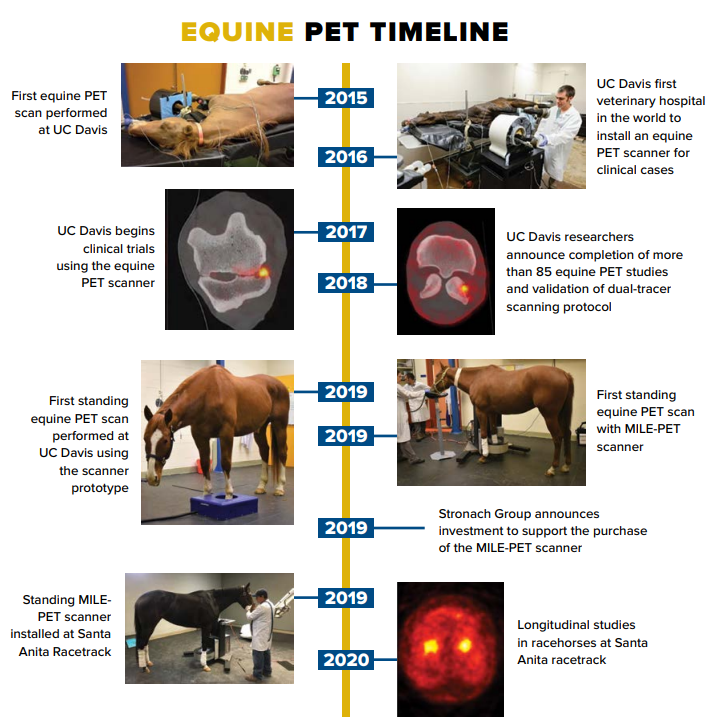
Image: digital, 3-dimensional, reflects physiologic changes
Best for: bone and soft tissue
Uses: lameness diagnosis, distinguish between active and inactive tendon lesions, regional differences in metabolic activity in hooves of horses with chronic laminitis
How it works: A positron-emitting radiotracer specific to bone or metabolic activity is injected intravenously (IV) into the patient. The radionuclide collects in areas of the body with higher levels of bone activity or greater metabolism and emits positrons. The emitted positrons interact with naturally occurring electrons in the body to yield gamma rays, which are detected by a ring of detectors around the patient. A computer analyzes the gamma rays and constructs three-dimensional images of the tracer concentration. CT images are typically acquired while the patient is still under anesthesia and the PET and CT images are fused for better assessment of the localization of lesions detected with PET.
How long it takes: 10-15 minutes per region
Pros: most sensitive technique to provide functional information, detects lesions not recognized with other imaging modalities, provides information at the molecular level regarding the activity of lesions, covers larger areas than MRI in the same amount of time, portable
Cons: limited to imaging of limbs, higher cost than other modalities
Cost: $$$
UC Davis standing equine PET scanner now in use at Golden Gate Fields
Standing Equine PET Now in Clinical Use at UC Davis
Equine PET: A Game Changer, Center for Equine Health Research Review
Positron Emission Tomography Performed on Standing Horse for First Time
